CAREGIVING TOOLBOX: Life Enrichment Visits
Aging in Place vs. Senior Living
Yes, senior living can be the answer for many when it comes to loneliness, but parents have the right to make decisions. We are very independent beings and many of our aging parents are not prepared to live in a senior living community. For them, aging in place is the best option.
Our response to this need and desire? A Life Enrichment program. Here’s what Caring Considerations will do to help reduce isolation.
We Want To Get To Know You
The in-person, Life Enrichment sessions are customized to meet the specific interests of seniors in ways that are meaningful and relevant. Clients typically receive weekly visits, but we will discuss a schedule to meet a loved-one’s desires.
What Are Life Enrichment Visits?
We provide hourly curated engagement, recreation, and social activities as part of a holistic Aging Life Care® plan.
Physical
- Workout buddy – PT prescribed exercises and seated exercise videos
- Walking Companion
Creative
- Writing
- Craft projects
- Reminiscing & conversation
Brain Fitness
- Math Brain Boost
- Trivia (variety of topics: sports, movies, country specific, holidays)
- Word puzzles
In our Aging Life Care® consulting practice, we witness numerous lingering issues resulting from the COVID lockdown. Older adults want to remain independent, but often lack the insight and energy to incorporate more social opportunities. The isolation imposed by the lockdown is perpetual and increasingly a barrier to seniors returning to the life they enjoyed prior to the pandemic.
An Added Benefit
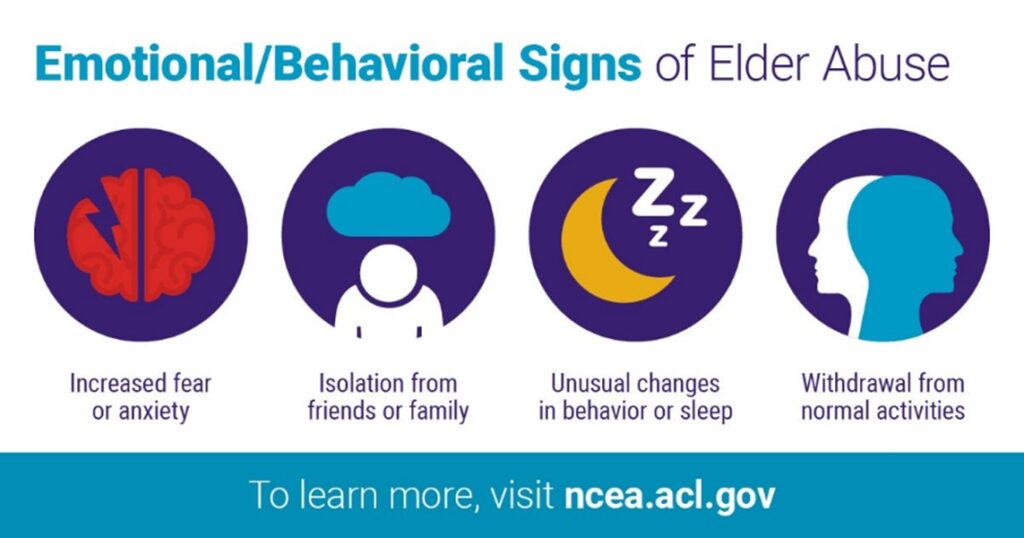
When your parent doesn’t want to move to assisted living, but you worry about them, Life Enrichment visits can be a non-threatening “check-in.” Although we don’t provide personal care, we can provide feedback about your loved one’s overall well-being.
Contact Us
To learn about this program and more, call 571-488-9396 or email us at [email protected].